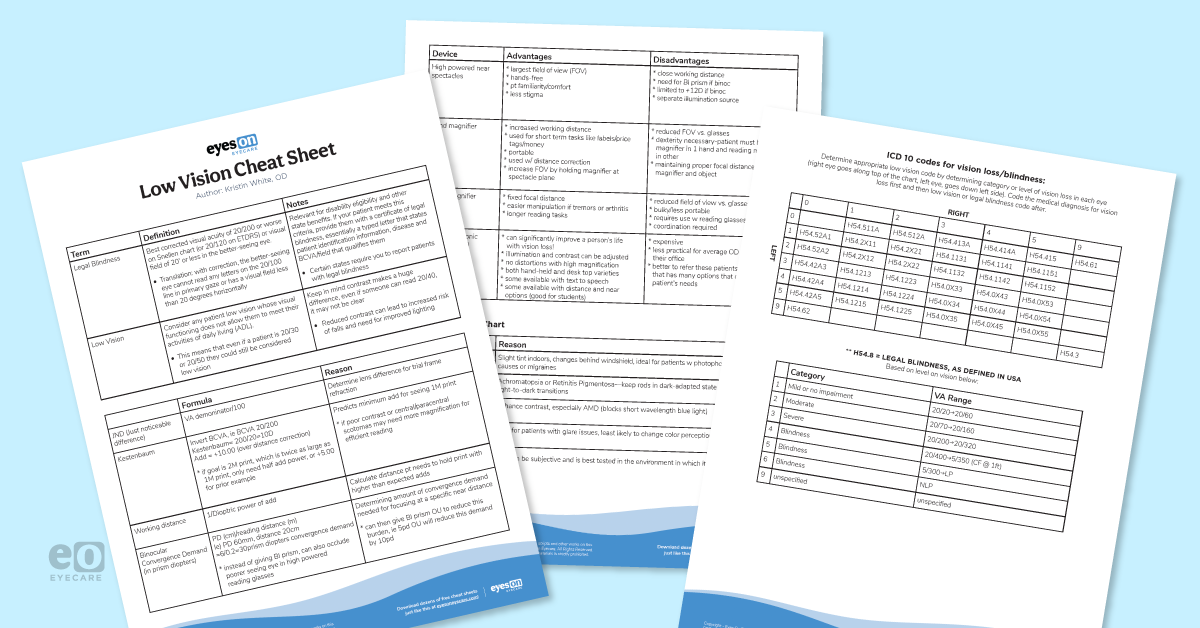
But first, download the cheat sheet!
Get the cheat sheet
Don’t forget, as soon as you are unable to meet your patients’ visual needs with the tools you have in your office, refer them to an optometrist who specializes in low vision. A patient with vision impairment can avoid years of frustration if they are referred to a low vision specialist early in their disease course. Low vision specialists can provide tools that can change with patients' visual needs, as well as give the patient hope for resources they can use if and when their vision worsens in the future.
A low vision exam is all about a thorough case history
- Ocular/medical hx; ocular surgeries/treatments
- Hx of vision loss: assess what patient knows about their vision problem and when they started/worsened
- ADL: occupation/avocation/living situation/driving
- Chief complaint & Goals: Ask specific tasks pt needs help seeing: ie) reading mail vs reading email vs loading insulin syringe—pt’s goals will help guide what tools you recommend
Low vision is about helping someone use the vision they have to do the things they need and want to do every day.
How to succeed in a low vision exam: notes from the (visual) field
- If reduced, the patient will need more magnification than based on VA alone
- Based on your patient's ocular disease, you will know whether they are likely to have reduced contrast (i.e., corneal scarring, cataracts, AMD all reduce contrast)
Trial frame refractions:
- Allows the patient to move their head around to use their eccentric viewing position
- Gives a more accurate representation of your patient’s vision in the real world
- JND = Just noticeable difference = amount of lens power needed to elicit an appreciable change = lens size difference made during refraction
- To calculate JND, use VA denominator and divide by 100
- i.e., if VA is 20/200, JND is 200/100 = 2.00 D, so show the patient +1.00/-1.00 in sequence during TF refraction; depending on which the patient prefers, remember the change you made was 2.00D in this example, so if the patient likes plus, you would add +2.00 over sph already in TF
- Use larger change JCC
- To determine minimum add (or amount of accommodation required) to read 1M print (average newspaper size print)
- Invert BCVA, ie BCVA 20/200 would then be 200/20 = 10 D
- Add = +10.00 (over distance correction)
- This can be manipulated depending on goal print size
- If the goal is 2M print, which is twice as large as 1M print, you only need half add power (or +5.00 for prior example)
- Working distance = 1/D = 1/10=0.1m (10 cm) working distance for above example
- Dioptric power can also be used to select magnification needed in hand or stand magnifiers (each magnifier is labeled with its dioptric value in addition to its magnification)
Keep in mind that patients can only read binocularly with about a maximum of +10.00 or +12.00D. If add needed is much greater than this, add should be applied to better functioning eye and occlude fellow eye so the patient can read monocularly.
Consider type of glasses
Consider fall risk
Have patience
Refer to a low vision specialist
- Technology training classes
- Orientation and mobility training
- Counseling (losing vision causes grieving just like any other loss)
- Other life skills classes