WHAT YOU'LL LEARN
The signs and symptoms of OIS
What to look for when diagnosing OIS
How carotid occlusive disease relates to OIS
How to treat and manage patients with OIS
Introduction
What is ocular ischemic syndrome?
Ocular ischemic syndrome (OIS) is characterized by hypoperfusion to the eye due to underlying systemic conditions, most commonly involving carotid artery disease. While this condition can also have sight-threatening ocular sequelae, it can have life-threatening systemic implications since carotid artery disease increases risk for stroke and cerebrovascular accidents. It is for this reason that eyecare providers must be able to quickly recognize OIS signs and symptoms in order to initiate the proper systemic work-up and treatment.1,2
Background information
As always, a thorough medical history and review of systems must be performed. The mean age of patients with OIS, as determined by Mizener et al., is 68 years-old, plus or minus a standard deviation of eight years. The condition is twice as common in men as women. Because patients who suffer from carotid occlusive disease often suffer from multiple comorbidities, it is always important to consider the appropriate differentials if not already diagnosed. According to Meziner et al.’s analysis of patients with OIS, more than 50% were diabetic, more than 50% had hypertension, 40% suffered from coronary artery disease and 30% had a history of stroke or transient ischemic attack.3
OIS is a rare condition. The proposed incidence is eight cases per million; however, considering underdiagnosis/misdiagnosis of the condition, experts note that this figure could be much greater.4 OIS retinal appearance can overlap with those of other conditions, such as diabetic retinopathy or retinal vascular occlusions. Making things even more difficult is the fact those other comorbidities are often detected and treated prior to a diagnosis of carotid occlusive disease. Carotid disease is often less obvious, and can be left undetected when OIS ocular signs are the only sign, as in more than half of cases.1
Signs and symptoms
The symptoms of ocular ischemic syndrome
The most common symptoms presented by a patient suffering from OIS are vision fluctuation or loss, and intermittent ocular pain. 90% of OIS cases report some type of vision disturbance.4 The vision loss presents as amaurosis fugax in approximately 15% of patients, gradual vision loss in 28% of patients, and sudden vision loss in 41% of patients. In a study conducted by Mizener et al., 64% of patients with OIS presented with visual acuity of 20/400 or less upon initial evaluation.3 The pain associated with OIS is described as dull, aching pain around and behind the orbit which may extend to the forehead and temple. 80% of OIS cases present with unilateral symptoms.4 The symptoms can be similar to those that present with Giant Cell Arteritis and thus this diagnosis needs to be ruled out in such cases.5
The signs of OIS
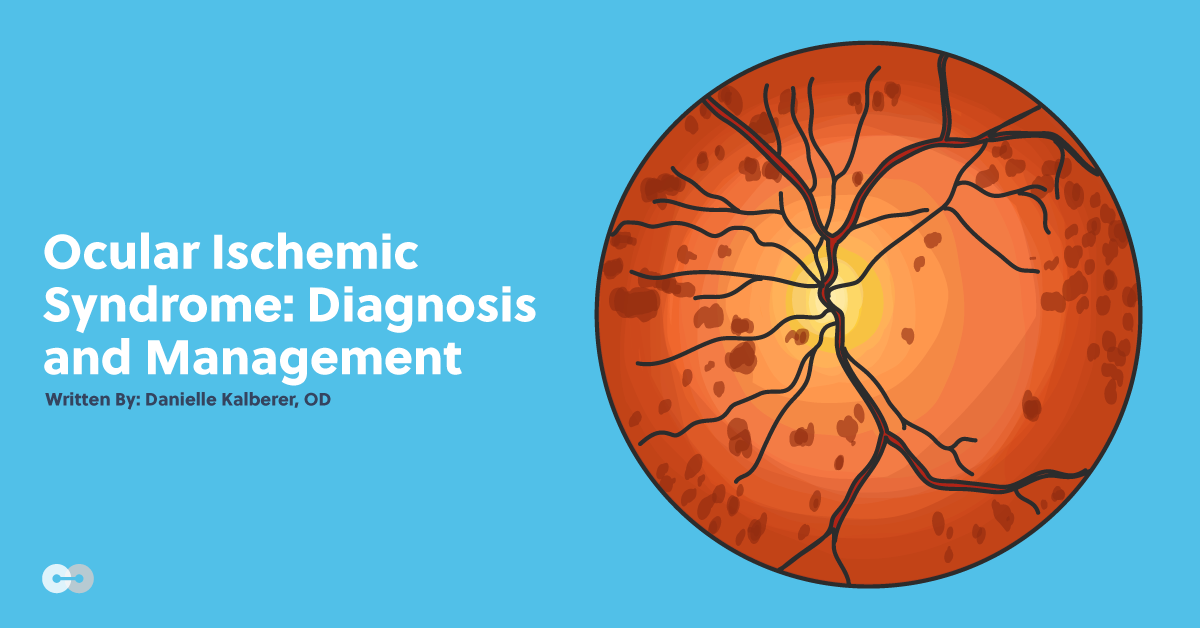
Clinical manifestations of OIS can involve both the anterior and posterior segment. The characteristic pattern of retinopathy associated with OIS is unilateral, mid-peripheral circumferential hemorrhages; characteristic hemorrhages are present in about 80% of cases. The hemorrhages are located in the more external retinal layers and often coincide with microaneurysms. Macular microaneurysms and telangiectasias can be present and lead to macular edema. In OIS, vascular changes demonstrating venous stasis and narrowing of arterioles are present and often associated with cotton wool spots.4
A major differentiating factor between central retinal vein occlusion and OIS is the presence of venous tortuosity in the former and lacking in the latter. A major differentiating factor between diabetic retinopathy and OIS is the presence of hard exudate with the former and lacking in the latter. It is important to remember that these differentials could co-exist, making the diagnosis more difficult.4
Optic nerve pallor or edema may be present due to hypoperfusion. According to Meziner et al., 40% of OIS patients presented with the former and 20% with the latter. Ischemic optic nerve disease can lead to optic atrophy consistent with normotensive glaucoma and neovascularization of the retina, optic disc, iris, and/or angle can ultimately develop into neovascular glaucoma in persistent cases.3,4 A sluggish mid-dilated pupil due to sphincter ischemia and prematurely advancing cataracts are also often noted in the afflicted eye. Dilated and prominent conjunctival and episcleral vessels may be noted and corneal edema in severe cases.4
Pathophysiology and Carotid Occlusive Disease
Carotid occlusive disease and ocular ischemic syndrome
OIS is a rare condition that is usually caused by severe occlusion of the carotid arteries. Atherosclerosis often leads to this condition.4
The ophthalmic artery is a branch of the internal carotid artery. The ophthalmic artery branches into the central retinal artery, short and long posterior ciliary arteries and the anterior ciliary arteries. Stenosis, most commonly caused by atherosclerosis, of the internal carotid reduces perfusion pressure within the central retinal artery leading to OIS.6 In addition to athlerosclerotic stenosis, other causes of OIS include systemic vasculitis, giant cell arteritis, trauma and inflammation. Because OIS is a manifestation of a systemic condition, it is imperative to enlist a cardiologist, vascular surgeon, and likely a neurologist in caring for these patients.
The mainstay of evaluating carotid occlusive disease is carotid duplex ultrasonography; a noninvasive imaging modality. According to Meziner et al., more than three quarters of OIS patients were found to have severe levels of stenosis in the 80-99% range on imaging studies.3 At hemodynamically significant stenosis levels the duplex study is specific but at levels less than 50% the specificity decreases. Additional testing options include computed tomography angiography (CTA) and magnetic resonance angiography (MRA).
High grade stenosis of the internal carotid does not guarantee OIS; the likelihood of OIS development is also dependent on the patient’s collateral circulation. With developed collateral circulation, there may be high grade carotid stenosis without OIS and with poorly developed collateral circulation there may be signs of OIS with only moderate grade carotid stenosis.4
Diagnostic testing
How to detect OIS in patients
Fluorescein angiography can be utilized to determine the extent of ischemia and differentiate between similarly presenting diagnoses such as vein occlusion. Injection-to-eye transit time of fluorescein dye can also suggest occlusive disease if delayed and/or asymmetric; an abnormal transit time can be observed in about 60% of patients.3,4 Automated visual field testing can be used to distinguish from other causes, such as non-arteritic ischemic optic neuropathy. OIS visual field results can range from normal, to centrocecal defects, to glaucomatous patterns if neovascular or normotensive glaucoma is a factor.4
Treatment and Management
Managing patients with OIS
After a diagnosis is confirmed by a combination of fluorescein angiography and carotid duplex, ocular treatments include conservative monitoring, laser or anti-VEGF injections and treatment with glaucoma therapy if indicated. Treatment with systemic medications entails anticoagulation agents, athlersclerotic therapy, hypertensive, diabetic, and heart disease treatment as indicated.
Carotid endarterectomy is the mainstay of treatment of carotid disease in prevention of stroke. The procedure involves the removal of athlersclerotic plaque from the common and internal carotids to restore blood flow. The North American Symptomatic Carotid Endarterectomy Trials (NASCET) established guidelines for the indications. The study results demonstrated the greatest benefit to those patients with 70-99% grade stenosis and history of ipsilateral stroke or transient ischemic attack. Treatment with carotid endarterectomy in this group was shown to decrease five year stroke and death rate by almost 30%.7 The Asymptomatic Carotid Artery Stenosis (ACAS) trial found that asymptomatic patients with greater than 70% should also be treated. Alternative options to endarterectomy are carotid stenting and angioplasty.2,4
Conclusion and References
In summary
Ocular Ischemic Syndrome is a rare, sight-threatening condition that can be the first and only hint of life-threatening conditions. The five-year mortality rate is about 40% after OIS onset, most likely from cardiovascular disease or stroke.4 This is why prompt diagnosis and referral to a vascular specialist are of the utmost importance. Test your knowledge of OIS with the quiz questions below.
References
- Mendrinos, Efstratios, et al. “Ocular Ischemic Syndrome.” Survey of Ophthalmology, vol. 55, no. 1, 2010, pp. 2–34., doi:10.1016/j.survophthal.2009.02.024.
- DaCosta M., Tadi P., Surowiec, S. M. Carotid Endarterectomy. StatPearls Publishing LLC, 2019.
- Mizener, Jane B., et al. “Ocular Ischemic Syndrome.” Ophthalmology, vol. 104, no. 5, 1997, pp. 859–864., doi:10.1016/s0161-6420(97)30221-8.
- Terelak-Borys, Barbara, et al. “Ocular ischemic syndrome - a systematic review.” Medical science monitor: international medical journal of experimental and clinical research vol. 18,8 (2012): RA138-144. doi:10.12659/msm.883260
- Grewal, Dilraj. S. “Ocular Ischemic Syndrome.” EyeWiki, 12 July 2019, https://eyewiki.aao.org/Ocular_Ischemic_Syndrome#Introduction.
- Kiel, Jeffrey W. The Ocular Circulation. Morgan & Claypool, 2011.
- Barnett HJ, et al. "Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis." The New England Journal of Medicine. 1998. 339(20):1415-25.
- Ho, Allen C., et al. “Color Doppler Imaging of the Ocular Ischemic Syndrome.” Ophthalmology, vol. 99, no. 9, 1992, pp. 1453–1462., doi:10.1016/s0161-6420(92)31784-1.